The nail diseases chart provided in this post will help you identify common nail disorders. The status of your nail can have a direct correlation with your overall well-being. A change in color, texture, or shape of your nail may be relatively harmless, but it may also be an indication of a disease. If you notice any of the changes mentioned in your fingernail or toenail, it is recommended that you schedule an appointment with a board-certified dermatologist.
Overview of Nail Diseases chart
Healthy nails are smooth and have consistent coloring. Vertical ridges or brittle nails may develop as you age. This is completely harmless. Spots caused by injury should fade as the nail grows. Discolored spots and nail separation can be caused by injuries to the fingers and hands, as well as infectious processes including warts (periungual warts), fungal infections (onychomycosis), and injury due to medications, such as those used for chemotherapy.
Certain medical conditions can also cause your fingernails to change color. These changes, however, can be difficult to interpret. The appearance of your fingernails is usually a clue to your underlying medical condition, but the doctor will make a diagnosis based on your nail findings, as well as after obtaining a thorough medical history.
Below is a chart representing common types of nail diseases with pictures:
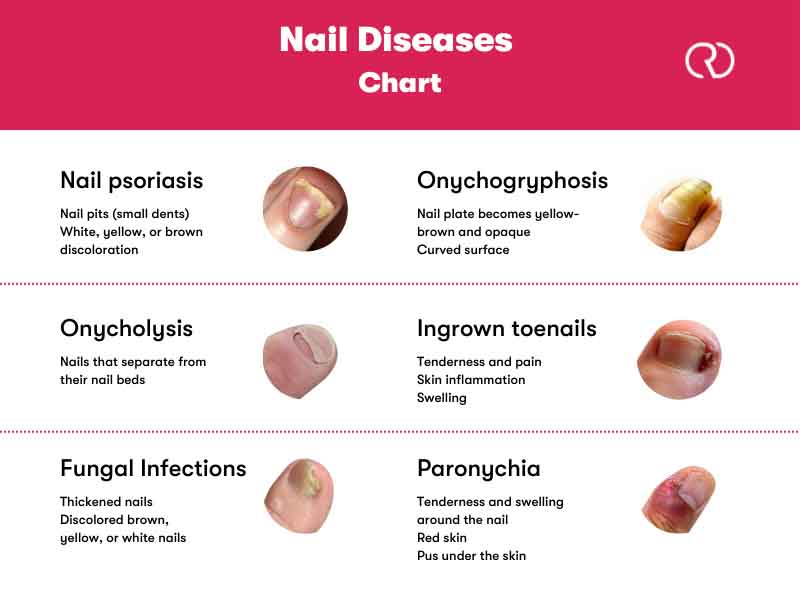
Common Nail Diseases
Fungal and bacterial nail infections are fairly common, as are nail disorders such as irregular splitting or abnormal color or texture. Poor hygiene, an unsuitable diet, genetics, tight shoes, and inefficient nail filing techniques can all contribute to nail problems.

When it comes to the most common nail conditions, the sooner you start treatment, the better—especially since nail abnormalities can help doctors detect underlying conditions.
A nail disease chart is provided below for each common nail disorder to help you better maintain your nail health.
Nail Psoriasis
Nail psoriasis is an autoimmune disease that causes discoloration, pitting, and changes in the structure of your nails. It can make you feel self-conscious, but you can improve their appearance by buffing them and applying nail polish. Nail psoriasis is not contagious, and treatments can help your symptoms improve.

| Underlying Causes |
|
| Symptoms |
|
| Treatments | Consult a dermatologist for the following options:
|
| At-home Care |
|
Can I catch nail psoriasis from another person?
Nail psoriasis does not spread. Skin-to-skin contact cannot transmit nail psoriasis to another person.
Onycholysis (Nail lifting up)
The separation of the nail from the nail bed is known as onycholysis. Onycholysis is a symptom of skin disease or skin infection, but it can also be caused by over-nail-filing, chemical exposure, allergic contact dermatitis, and other injuries. Onycholysis can lead to infections and permanent nail loss if not treated and cared for properly during the healing process.

| Underlying Causes |
|
| Symptoms |
|
| Treatments |
|
| At-home Care |
|
Is Onycholysis painful?
Onycholysis nail disorder is usually not painful; however, the cause of your onycholysis may be painful or irritating. Onycholysis caused by injuries or fungal infections can cause pain and irritation.
Can I catch Onycholysis?
Onycholysis caused by an injury, nail psoriasis, or a reaction to a medication or chemical is not contagious. Onycholysis caused by a fungus, on the other hand, could be contagious. Skin-to-skin contact between infected individuals can spread the fungus. Nail fungus can also be contracted by touching an infected surface (indirect contact).
Nail Fungal Infections
Next on the nail diseases chart is nail fungus, which is a common nail infection. It starts as a white or yellow-brown spot under the tip of your fingernail or toe. As the fungal infection progresses, the nail may discolor, thicken, and crumble at the edge. Nail fungus can affect fingernails, but it is more common in toenails. In addition to being an infectious condition, nail fungus causes great discomfort.

| Underlying Causes |
|
| Symptoms |
|
| Treatments |
|
| At-home Care |
|
When should I see a doctor for a nail fungal infection?
If self-care measures haven’t helped and the nail becomes increasingly discolored, thickened, or misshapen, you should see a doctor. In the event that you experience any of the following signs, see a dermatologist:
- You have diabetes and believe you have nail fungus.
- The skin around the nails is bleeding
- Swelling or discomfort near the nails
- Having trouble walking
Onychogryphosis (Ram’s Horn Nails)
Onychogryphosis is a nail condition in which one side of the nail grows faster than the other. This disease is known as “ram’s horn nails” because the nails are thick and curvy, similar to horns or claws. Onychogryphosis primarily affects the toes, particularly the big toe.

| Underlying Causes |
|
| Symptoms |
|
| Treatments |
|
| At-home Care |
|
Ingrown toenails
Ingrown toenails occur when the corner or side of a toenail grows into the soft flesh. As a result, there is pain, inflamed skin, swelling, and, in some cases, infection. Ingrown toenails are most commonly found on the big toe.

| Underlying Causes |
|
| Symptoms |
|
| Treatments |
|
| At-home Care |
|
Can an ingrown toenail heal on its own?
Minor ingrown toenails can heal naturally as the nail grows. Ingrown nails that are severe or infected, on the other hand, require professional medical attention. It’s critical to understand the symptoms of an ingrown nail infection, so you know when to seek medical attention.
Paronychia (Nail Infection)
The most common cause of paronychia (nail inflammation) is a bacterial infection. Cuticle and nail fold cuts allow bacteria to enter the skin (the skin around the nail). Antibiotics are effective in treating most nail infections. Typically, paronychia doesn’t result in significant health issues. The infection can occasionally persist for a long time or recur after treatment.

| Underlying Causes |
|
| Symptoms |
|
| Treatments |
|
| At-home Care |
|
What are the different types of paronychia?
Paronychia is classified into two types. Both types have the following signs and symptoms:
- Acute paronychia: Acute paronychia symptoms appear over a few hours or days. The infection is limited to the nail fold and does not spread further inside the finger or toe. Symptoms resolve in less than six weeks with treatment.

- Chronic paronychia: Symptoms appear more slowly than acute paronychia and last for six weeks or longer. Several fingers or toes can become infected at the same time. Along with the bacterial infection, a nail fungus (usually caused by a fungus called candida) may develop. Candida is one of several fungi that can cause fungal infections in the toes.

Bottom line About Nail diseases
The present nail diseases chart was designed with the goal of helping you recognize common types of nail disorders, symptoms, causes, and how to treat them. Preventing nail diseases generally comes down to proper hygiene, a nutritious diet, and regular maintenance of the nails.

Take into account consulting a medical expert about potential underlying nail diseases if you experience any unexplained symptoms. The majority of the underlying causes of nail problems are simple to address once they are discovered.
You can get more information about online dermatology consultation by click on the link.
As discussed in this nail diseases chart, nail disorders are challenging to treat and can be frustrating for both patients and clinicians. Because of the slow growth rate of the nail plate and the difficulty of getting medications to penetrate into the nail tissues, treatment results are usually delayed for several months.

2 comments
I have heard that there is a relationship between nail diseases and overall health. is that right?
Yes, there can be a connection between nail diseases and overall health. For example, nail fungal infections can be a sign of a weakened immune system.