Skin cancer is the most common type of cancer and affects a wide range of people. Extra ultraviolet (UV) light exposure, whether from the sun or other sources such as tanning beds, is the leading cause of skin cancer. Rashes, blisters, and moles can all be symptoms of skin cancer. This post will go into detail about skin cancer and how it develops. In addition, we will provide detailed information on various skin cancer types, rashes, and treatments.
What exactly is skin cancer?
Skin cancer is the uncontrolled growth of abnormal cells in the epidermis (the outermost skin layer) caused by unprepared DNA damage that yields mutations. These mutations result in skin cells multiplying rapidly and forming malignant tumors.
Sun-exposed skin is the most vulnerable to skin cancer. However, this common type of cancer can develop in areas of your skin that are not normally exposed to sunlight.
As ozone levels deplete, the atmosphere’s protective filter function deteriorates, and more solar UV radiation reaches the Earth’s surface. A 10% reduction in ozone levels is expected to result in an additional 300,000 non-melanoma and 4,500 melanoma skin cancer cases.
By limiting or avoiding your exposure to ultraviolet (UV) radiation, you can lower your risk of developing skin cancer. Checking your skin for suspicious changes can help in the detection of skin cancer in its early stages. Early detection of skin cancer improves your chances of successful treatment.
If you are exposed to sunlight for extended periods of time, Actinic keratoses should not be overlooked. Also known as solar keratoses, actinic keratoses are sun-damaged dry scaly patches of skin. The patches are usually not serious, however, there is a small chance that they will develop into skin cancer, so it is critical to avoid further damage to your skin.
According to the World Health Organization (WHO), globally, there are between 2 and 3 million non-melanoma skin cancer cases and 132,000 cases of melanoma. Additionally, statistics from the Skin Cancer Foundation indicate that one in five Americans will develop skin cancer in their lifetime, and one in three cancers that are diagnosed are skin cancers.
Skin Cancer Types
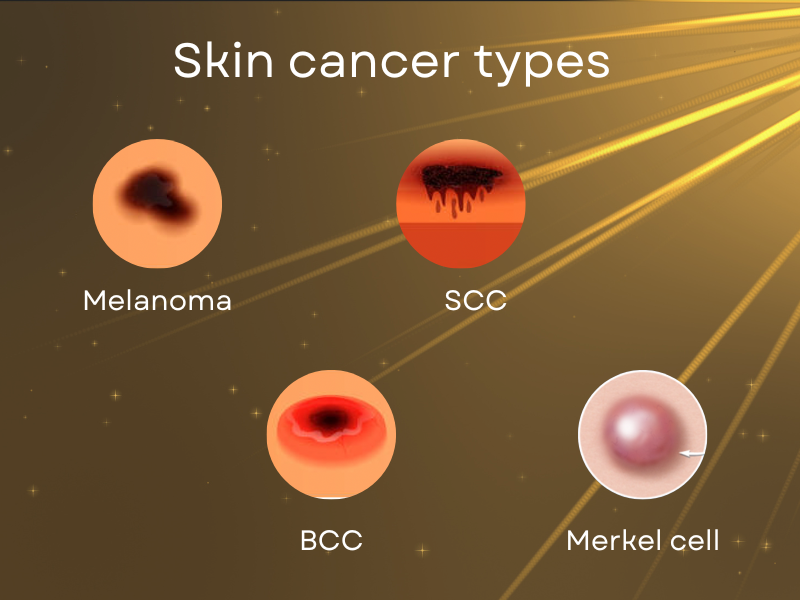
The four main skin cancer types are as follows:
- Basal Cell Carcinoma (BCC): Basal cells are the round cells found in the lower epidermis. About 80% of skin cancers develop from this type of cell. Basal cell carcinoma can be found anywhere on the skin, but it typically appears on the head and neck. It primarily results from sun exposure or manifests in patients who had radiation therapy in childhood.
- Squamous Cell Carcinoma (SCC): Squamous cells are flat, scale-like cells that make up the majority of the epidermis. Squamous cell carcinoma is primarily caused by sun exposure but can occur anywhere on the skin. It can also appear on skin that has been burned, damaged by chemicals, or exposed to x-rays. Lips, areas where a scar has been present for some time (chronic wound), and the anus (exposed to HPV) are common areas for squamous cell cancer.
- Merkel cell cancer: Highly aggressive or rapidly spreading, Merkel cell cancer is a rare type of cancer. It starts in the hair follicles and in the hormone-producing cells under the skin and usually affects the head and neck area. Merkel cell carcinoma is also referred to as neuroendocrine carcinoma of the skin.
- Melanoma: Melanocytes, which are sporadic cells, are present where the epidermis and dermis meet. The pigment melanin, which gives skin its color, is produced by these cells. The most aggressive form of skin cancer is melanoma, which begins in melanocytes and causes about 1% of all skin cancers.
Non-melanoma skin cancer can also take the form of sarcomas, skin adnexal tumors, Kaposi sarcomas, and cutaneous (skin) lymphomas, all of which are less common.
What do they look like?
Different skin cancers have different symptoms associated with them which includes rashes, blisters, bleeding, or being itchy.. Most common skin cancer are as follows:
Basal cell carcinoma (BCC)
The typical outward sign of basal cell carcinoma (BCC) is a small, shiny pink or pearly-white lump that has a translucent or waxy appearance. It may also resemble a scaly, red patch. Sometimes the patch contains some brown or black pigment.
Squamous Cell Carcinoma (SCC)
Squamous cell carcinoma presents as scaly red or skin colored bumps that tend to be painful, itchy as well as bleeding at times. It is more common at the area which has significant sun exposure including lips, ear, forearm, chest and face area. In individuals with thinner hair, SCC can develop over their scalp area.
Merkel cell cancer
Merkel cell carcinoma (MCC) is a rare skin cancer that appears to be very aggressive. It can be misdiagnosed as an insect bite, cyst, or even a pimple.This type of skin cancer usually appears as a sore on the head or neck. Because MCC is so aggressive, detecting it early can save a person’s life. MCC has the following characteristics that can help you detect it early:
- Appears on the head or neck (mostly, but it can be present anywhere else too)
- Rapid expansion
- Is red, purple, or pink
- Not painful
- Appear after the age of 50
Melanoma
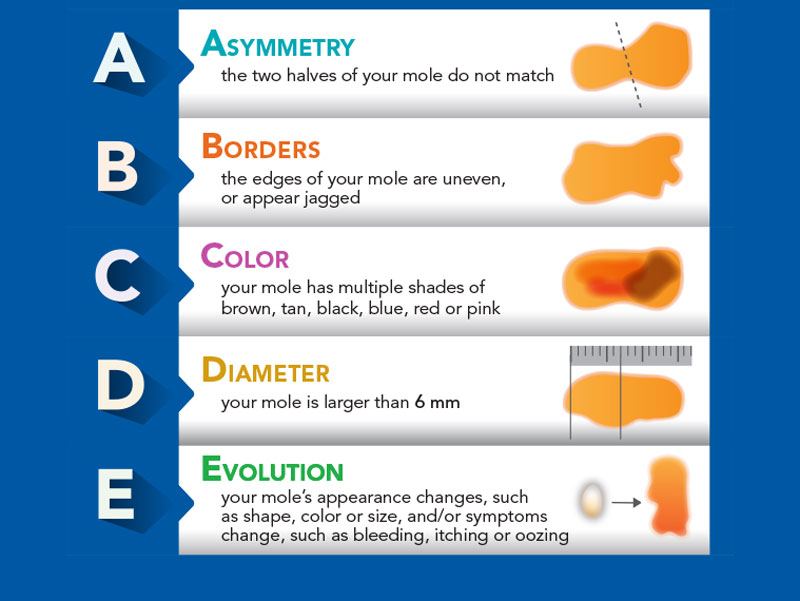
A change in the shape, color, size, or feel of an existing mole is frequently the first sign of melanoma. Melanoma, on the other hand, can manifest as a new mole. Of course not every mole is melanoma, however, if the mole has the following characteristics, consult a dermatologist:
ABCDE of Melanoma:
- There is no symmetry (it is asymmetrical)
- In outline, the borders are frequently ragged, notched, or blurred. The pigment may spread into the skin around it.
- Shades of black, brown, and tan are possible. There may also be white, gray, red, pink, or blue areas. Different colors associated with the mole.
- The diameter of the lesion has increased. Melanomas can be very small, but most are larger than a pencil eraser (more than 6 millimeters or about 1/4 inch).
- The mole has changed in recent weeks or months. There is evolution associated with it.
Facts and lies about skin cancer
There are many facts and myths that circle around the internet about skin cancer, but how to make sure which of them are true? Below, we have consulted dermatologists for the most common facts and myths about skin cancer:
- Skin cancer is NOT solely carried on by sun exposure
Skin cancer is primarily brought on by sun exposure, but there are other factors playing important roles as well:
- Exposure to ultraviolet (UV) radiation from sun beds and work tools
- Genetic factors including history of skin cancer
- Immunosuppressed stats
- Certain medication as well as x-ray radiation can increase chance of specific types of skin cancer
People with fair skin, freckles, and multiple or unusual moles are at a higher risk of developing skin cancer.
- Sunburns DO cause skin cancer
The DNA of your skin cells is damaged when ultraviolet rays from the sun or a tanning booth strike it. Your body sends melanin, or pigment, to the surface of your skin to protect your cells. As a result, your skin becomes tanned due to UV exposure.
Tanning is the direct result of your skin damage to UV radiation, according to dermatologists. Your body’s skin cells are doing everything they can to prevent further damage, but it won’t be enough if you continue exposing your skin to harmful UV radiation.
The minor protective effect of a tan can be easily wiped out by additional UV exposure, resulting in further damage. Sunburn occurs when the UV rays are too strong for the skin to handle and repair.
- Risk of developing skin cancer can be inherited
Researchers have discovered that certain defective genes can be passed down through generations. This increases your chances of developing skin cancer. According to the American Cancer Society, DNA changes in tumor suppressor genes, such as CDKN2A and BAP1, can increase your risk of melanoma. It is estimated that 5 to 10% of melanoma cases are hereditary and caused by a pathogenic gene variant or change in a gene sequence.
- You CAN get UV exposure while being indoors
Sun protection is necessary because both direct and indirect UV rays cause skin damage. Dermatologists have discovered that even brief exposure to sunlight throughout the year can cause significant damage to your skin especially in individuals with fair skin.
These brief moments can include driving with the sunroof open or walking around in outdoor shopping centers between 10 a.m. and 4 p.m. when sun radiations are at its peak.. These cumulative, everyday exposures have been linked to different types of skin cancer but particularly with squamous cell cancer. Window film shields against harmful UV rays at home, work, and on the road can be very beneficial in reducing risk of skin cancer.
There are numerous myths about melanoma and skin cancer in general. Because no one is immune, it is critical to examine your skin from head to toe every few months. Consult a dermatologist if you notice a new mole or a change in an existing mole.
Signs & Symptoms of Skin Cancer
The most common sign of skin cancer is a change in your skin. This could be a new growth, an unhealed sore, or a change in a mole. It is important to note that not all skin cancers have the same appearance.
Basal Cell Carcinoma (BCC)
Symptoms:
Small, shiny bumps or nodules that are red, pink, or white; persistent non healing sore; reddish flat patch; or a scar-like white or yellowish area
Progression:
Grows slowly and will bleed, crust over, and then cycle repeats.
Treatment:
surgery to remove all of the cancer and some of the surrounding healthy tissue
Squamous Cell Carcinoma (SCC)
Symptoms:
Red, scaly patches or bumps
Progression:
Can develop into large masses
Treatment:
Squamous cell carcinoma, especially those classified as high risk, is frequently removed surgically
Merkel cell cancer
Symptoms:
Typically a painless, firm bump that can be red-purple or skin-colored on sun-exposed skin (such as the head, neck, and arms).
Progression:
a tendency for rapid growth and early metastasis (spreading).
Treatment:
Immunotherapy is most commonly used to treat Merkel cell carcinoma that has spread to other parts of your body.
Melanoma
Symptoms:
Asymmetrical, mottled patches with notched or blurred borders, typically in tan, brown, or black
Progression:
Can appear without warning, or may begin in or near a mole or other dark spot on the skin.
Treatment:
The primary treatment for all stages of melanoma is surgery to remove the tumor. Skin grafting may be used to cover a surgical wound.
Symptoms of basal cell carcinoma
Basal cell carcinoma (BCC) is mostly found in sun-exposed areas of the body, such as the neck or face. A pearly or waxy bump, a flat, flesh-colored lesion, and bleeding or scabbing sore that heals and scabs again are all signs of BCC skin cancer.
Symptoms of Squamous Cell Carcinoma
Squamous cell cancer may appear as a firm, red nodule or a flat lesion with a scaly, crusted surface. The spot tends to be very scaly, bleeding and painful at times. It doesn’t resolve without any active treatment.
Symptoms of Melanoma
Melanoma can develop anywhere on your body. It can develop from sun damaged skin or arises from an existing mole. It most commonly appears on the face or trunk of affected men, and it develops on the lower legs of affected women.
Melanoma signs include: A mole which is a substantial brownish spot with darker speckles that bleeds, and changes in size, color, or texture; A painful lesion that itches or burns; a small lesion with an irregular border and areas that appear red, pink, white, blue, or blue-black; dark lesions on the mucous membranes lining your mouth, nose, vagina, or anus.
The “A-B-C-D-Es of melanoma” is an easy way to remember the warning signs for this particular skin cancer:
- Asymmetrical: Does the mole or spot have two parts that are very different in appearance and have an irregular shape?
- Border: Is the border ragged or erratic?
- Color: Is the color inconsistent?
- Diameter: Is the mole or spot bigger than a pea in size?
- Evolving: Have there been any recent changes to the mole or spot?
Skin Cancer Treatment
The majority of skin cancers are basal cell or squamous carcinomas, which can be treated at a dermatologist’s office. However, more aggressive skin cancers, such as melanoma or Merkel cell carcinoma, typically require more extensive treatment such as surgery, chemotherapy, and immunotherapy.

Below, we’ll undercover more detail about each of these skin cancer treatment methods:
- Surgery
Surgery to remove the entire tumor may be the only course of treatment required for skin cancers that have not spread. More complex surgeries might be necessary for skin cancers that are more aggressive, like melanoma. If nearby lymph nodes are enlarged and the doctors suspect cancer cells have spread, they might decide to remove them. Typical surgical skin cancer treatment approaches include:
- Mohs surgery
Mohs surgery is most commonly used on more visible areas of the body, such as the head and neck or the hands. Dr. Frederick Mohs developed this technique in the 1930s to remove skin cancer tumors while preserving as much healthy tissue as possible. It could commonly be used to treat recurring skin cancers.
Recommended Article : What Exactly Does a Dermatologist Do for Your Skin?
- Cryosurgery
This technique, also known as the freezing method, uses liquid nitrogen to freeze and destroy cancer cells. This is typically reserved for minor skin cancers or precancerous lesions. After the wound heals, the treated area may swell, blister, and scar.
- Excision
In this method, the surgeon performs an excision with a scalpel or sharp razor, cutting or shaving the growth off the skin. To numb the affected area, the patient may be given local anesthesia. Excisions can leave a scar, and surgeons can perform a variety of excisions:
A simple excision is made by removing the skin growth and a small perimeter of surrounding tissue with a scalpel.
Shave excision is a procedure in which the growth on the skin’s surface is shaved or peeled away with a sharp razor-like tool.
A wide excision removes the skin tumor as well as a larger perimeter of healthy tissue. A broad excision may also go deeper into the skin than a simple excision. This surgery is commonly used to treat melanomas and Merkel cell carcinomas.
- Reconstructive surgery
Scarring or disfigurement may result from skin cancer surgery, particularly when a wide excision or other extensive surgery is required to remove skin cancer, or when the surgery is performed on the face, head, neck, or hands.
- Curettage and electrodessication
A curette is a long, thin surgical instrument with a small, sharp hoop or scoop at one end for scraping. Following scraping of the lesion, the area is treated with an electric current delivered through a needle-like electrode designed to kill remaining cancer cells and reduce bleeding. This is known as electrodesiccation. It may require a local anesthetic and leave a scar.
- Laser surgery
This methodology uses a laser beam to destroy cancer cells. Laser surgery may be used to treat skin cancers that are very superficial.
- Lymph node biopsy and removal
Melanoma patients are frequently subjected to a lymph node biopsy. If the melanoma is deeper than 0.75 mm or it is ulcerated then sentinel lymph node (SLN) biopsy would be offered. SLN is the first lymph node that drains the lymphatic system from the site where melanoma was discovered. if no evidence of cancer is found in the lymph nodes or nodes, no further lymph node surgery is required. If melanoma cells are discovered in one or more sentinel lymph nodes, the surrounding lymph nodes may be removed.
- Topical treatments
Non-surgical treatments may be used in some cases to remove or destroy localized skin cancer cells. Treatments for superficial basal cell or squamous cell carcinomas in situ (stage 0), as well as noncancerous or precancerous lesions, fall into this category. The following are examples of topical treatments.
- Photodynamic therapy
This method entails directly applying a light-sensitive substance, typically aminolevulinic acid (Levulan®), to the tumor and exposing it to a special blue light that targets cancer cells. This treatment is most commonly used on actinic keratoses, which are precancerous growths that, if left untreated, can develop into squamous cell carcinomas.
The most common side effect of photodynamic therapy is light sensitivity. Patients should consult their doctor about the duration of their light sensitivity.
- Topical chemotherapy
Basal cell carcinoma and actinic keratoses can both be treated with topical chemotherapy. This treatment involves applying a chemotherapy cream, typically fluorouracil (Efudex®), directly to the skin tumor. The application can be done twice daily for as little as three weeks or as long as twelve weeks.
Fluorouracil can cause an allergic reaction in rare cases. If patients experience severe side effects such as fever, difficulty swallowing, or digestive issues, they should seek medical attention.
- Immune response modifier
The topical cream imiquimod (Zyclara® Aldara®) may be used to treat actinic keratoses or superficial basal cell carcinomas. Application may be prescribed several times a day for two to eight weeks. It works by stimulating the body to produce interferon, a natural protein that fights foreign invaders and cancer cells.
An immune response modifier’s side effects could include skin that is red, itchy, bleeding, or flaking, swelling, stinging blisters, pain, fatigue, exhaustion, back pain, headache, or diarrhea.
- Chemotherapy
Chemotherapy is a crucial component of the treatment of skin cancer, particularly if the disease has spread to distant organs. Basal cell carcinoma that has spread locally may be treated with topical chemotherapy. Chemotherapy frequently has side effects, which can include digestive problems, hair loss, and immune system suppression.
- Radiation therapy
Radiation therapy may be used to treat skin cancer, especially if the cancer has spread to the brain or bones. It can also be used after surgery to treat affected lymph nodes, to destroy any remaining cancer cells and to reduce the size of the metastases in the body. Radiation therapy techniques used to treat skin cancer include those below:
- External beam radiation therapy (EBRT)
A radiation beam is directed at cancerous tissues inside the body during external beam radiation therapy (EBRT). Radiation doses are adjusted to destroy cancerous cells and reduce tumor size.
- Intensity modulated radiation therapy (IMRT)
Intense modulated radiation therapy (IMRT) may be an option for you if you have had previous radiation therapy for skin cancer. IMRT allows radiation oncologists to use higher radiation doses than traditional therapies would allow in certain areas of the body. It also helps to spare more of the surrounding healthy skin tissue from harmful doses of radiation.
Preventing skin cancer
In order to prevent skin cancer, you must take a comprehensive approach to shielding yourself from dangerous UV radiation. This is due to the fact that UV radiation from the sun is not only harmful, but also cunning. Even when you try to avoid it, it can penetrate clouds, and bounce off of snow, water, and sand, leading to premature aging and skin cancer. Additionally, sun damage builds up over time from simple activities like walking around the neighborhood, driving the kids to the school, and taking out the trash, as well as from prolonged outdoor exposure.

The American Academy of Dermatology Association (AAD), recommends you to follow these steps to prevent skin cancer:
- When necessary, seek shade, keeping in mind that the sun’s rays are most intense between 10 a.m. and 4 p.m.
- When possible, dress in UV-protective clothing such as a light, long-sleeved shirt, pants, a wide-brimmed hat, and sunglasses. For better sun protection, wear clothing with an ultraviolet protection factor (UPF) label.
- Use a water-resistant, broad-spectrum sunscreen with an SPF of 30 or higher. Both UVA and UVB rays are protected by broad-spectrum sunscreen.
- Even on cloudy days, apply sunscreen wherever you go outside.
- Apply enough sunscreen to cover any exposed skin that is not covered by clothing. To fully cover their bodies, most adults require about 1 ounce, or enough to fill a shot glass.
- Remember to apply sunscreen to the tops of your feet, neck, ears, and top of your head.
- When spending time outside, reapply sunscreen every two hours, or after swimming or sweating.
- Water, snow, and sand should be avoided because they reflect the sun’s harmful rays, increasing your chances of getting sunburned.
- Stay away from tanning beds. Skin cancer and premature aging of the skin can be brought on by ultraviolet light from tanning beds.
- If you want to look tan, consider using a self-tanning product, but keep applying sunscreen while using it.
- To be able to detect skin cancer early, when it is most treatable, perform routine skin self-exams. If you notice any new or suspicious spots on your skin, or anything changing, itching, or bleeding, consult a board-certified dermatologist.
Nicotinamide can help prevent certain skin cancers
It has been demonstrated that the vitamin B3 compound nicotinamide lowers the incidence of skin cancer. A randomized controlled trial conducted in Australia and reported in the New England Journal of Medicine found a 23% reduction in the risk of basal cell and squamous cell carcinoma. When exposed to sunlight, ultraviolet damage is protected by nicotinamide.
The vitamin is safe and can be purchased without a prescription. All of those patients who had a history of basal cell carcinoma or squamous cell carcinoma, or who had extensive sun damage are advised to consult a dermatologist to begin taking the vitamin.
Benefits of TeleDermatology in Diagnosing Skin Cancer
Telehealth is being widely used by healthcare professionals to diagnose and treat skin cancer. Technologies like smartphones, tablets, and computers are widely used in delivering healthcare. It can also make it easier for people to access specialized care if they live in remote areas.
Dermatologist can review skin spots using TeleDermatology and potentially making diagnosis based on images. However, it is still required for the patient to be seen in clinic for possible skin biopsy as well as thorough skin examinations. Telehealth visits are intended to fill in the gaps between your regular dermatologist’s visits rather than replace your yearly skin examinations. You can schedule online appointments with dermatologists in the following circumstances:
New Skin Growth
If you notice a new skin growth or a sore that does not seem to heal, you should consult a dermatologist. Because much of a dermatology skin screening is visual, your dermatologist can take a look at the growth if you send them photos.
They can include: a new spot that appears to be growing; a sore or blemish that never heals; a rough, scaly patch of red skin; a mole that is changing its size or shape.
Follow-Up Visit
To follow up with you after skin cancer treatment, many dermatologists can now offer telehealth appointments. Your dermatologist might be able to virtually assess your surgical site as long as it is healing well and showing no signs of infection. Most likely, a video visit and pictures of the location will be requested by your doctor.
Informational Appointment
Your type of skin cancer, prognosis, and treatment plan may be discussed during a virtual appointment. It could be with your primary care physician or another healthcare professional, such as a nurse practitioner, or physician assistant. Many dermatologists can provide educational services without the need for in-person visit.
What conditions increase the risk of getting skin cancer if not treated?
- Abnormal moles
People who have a lot of moles or abnormal moles called dysplastic nevi are more likely to get skin cancer. These abnormal moles, which appear irregular and are generally larger than normal moles, are more likely to become cancerous than others. If you have a history of abnormal moles, keep an eye out for changes.
- A weak immune system
People with weakened immune systems are more likely to develop skin cancer. This includes people living with HIV/AIDS and those on immunosuppressive medications following an organ transplant.
- Excessive sun exposure
Anyone who spends a significant amount of time in the sun is at risk of developing skin cancer, especially if their skin is not protected by sunscreen or clothing. Tanning, including tanning lamps and beds, puts you at increased risk. Tans are your skin’s injury response to too much UV radiation.
- A history of sunburns
If you had one or more blistering sunburns as a child or teenager, you are more likely to develop skin cancer as an adult.




6 comments
Hi thank you for the article. can a normal skin tag turn into cancer?
Hello noth. Actually skin tags are extremely rare to become precancerous or cancerous, however if your skin tag changes color or shape, you should consult your dermatologist.
Is skin cancer hereditary? Can it pass from parents to children?
Hi Erika. Family history is a risk factor for skin cancer. One in ten patients with melanoma has a family member with the disease. You are more likely to develop melanoma if you have a direct biological relative who has/had it – your parents, siblings, brothers, or children.
Hi there, I have a mark like “Merkel cell cancer” in your article., i am so afraid now and I want a doctor to check it, is it possible online?
Hello Nina! Please keep calm, we’re here to help. If you create a case on RemoteDerm, you can upload photos of your skin condition to be diagnosed by a board-certified dermatologist. You will be informed if further action needs to be taken at a local dermatologist’s office.