Ringworm is a common fungus-caused skin infection. It is characterized by a red, itchy rash in both humans and animals. It can be difficult to identify because it is frequently confused with other skin conditions. This article will go over the causes of ringworm, as well as its symptoms, treatments, and prevention tips. We will also discuss how to diagnose ringworm and when you should see a doctor. So, if you suspect you are suffering from ringworm, keep reading to find out what to do.
What is Ringworm?
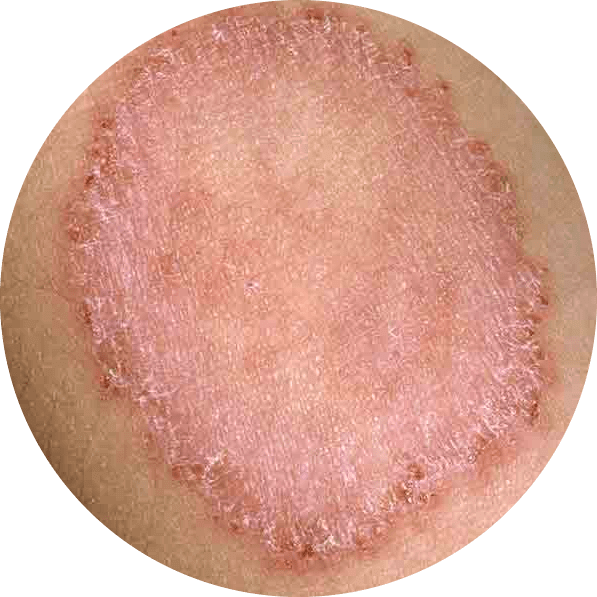
A fungal infection that causes a rash is ringworm of the body (tinea corporis). It typically manifests itself as an itchy, circular rash with clearer skin in the center. Ringworm is named after the way it appears. There is no actual worm present. Athlete’s foot (tinea pedis), jock itch (tinea cruris), and scalp ringworm are all associated with ringworm (tinea capitis).

Ringworm is most commonly transmitted through direct skin-to-skin contact with an infected person or animal. Topical antifungal medications are frequently effective in treating mild ringworm. Antifungal pills may be required for several weeks for more severe infections.
Ringworm Symptoms
As mentioned, the most common symptom of ringworm is a red, itchy rash that often has a circular shape with raised, scaly edges. It may also be accompanied by blisters or pus-filled bumps. The rash can appear anywhere on the body but is most common on the scalp, feet, and groin area.
Other symptoms of ringworm include:
- Itching
- Burning sensation
- Flaking skin
- Discolored patches of skin
- Cracked or thickened nails
Ringworm symptoms on different body parts:
- Scalp (tinea capitis): Ring worm on the scalp is typically characterized by a scaly, itchy, red, circular bald spot. If the infection spreads, the bald spot may grow in size and multiple spots may appear. Ringworm of the scalp is more prevalent in children than in adults.
- Beard (tinea barbae): Scaly, itchy, red spots on the cheeks, chin, and upper neck are signs of ringworm in the beard. The affected hair may bald, and the spots may become crusted over or pus-filled.
- Feet (tinea pedis or “athlete’s foot”): Red, swollen, peeling, itchy skin between the toes is one of the signs of ringworm on the feet (especially between the pinky toe and the one next to it). The foot’s heel and sole may also be impacted. In severe cases, blisters can form on the skin of the feet.
- Groin (tinea cruris or “jock itch”): Ringworm on the groin appears as scaly, itchy, red spots on the inner sides of the thigh skin folds.
Causes of Ringworm
The fungus that causes ringworm is spread through direct contact with infected people, animals, or objects. It can also be picked up from contaminated surfaces, such as locker rooms, showers, or swimming pools. This makes it important for individuals to practice good hygiene in order to reduce the risk of contracting ringworm.
The fungus thrives in warm, moist environments. It can also be spread through contact with contaminated items, such as clothing, bedding, or towels. It is important to note that ringworm is not caused by worms and does not always take the shape of a circle.
Risk Factors
Anyone can develop ringworm, but some people are more at risk than others.Those who have the following circumstances are more likely to develop body ringworm:
- People living in warm climates
- Those in close proximity to an animal or person who is infected
- a person who shares towels, linens, or clothing with a person who has a fungal infection.
- one who engages in contact sports, such as wrestling, where there is skin-to-skin contact.
- those who wear clothing that is too tight or restrictive.
- People who have a weakened immune system
Treating a Ringworm Rash
The treatment for ringworm is determined by its location on the body and the severity of the infection. Some types of ringworm can be treated with non-prescription (“over-the-counter”) medications, but others require prescription antifungal medication. Prescription medications can include topical creams, ointments, or oral antifungal pills.

- Ringworm on the skin: Non-prescription antifungal creams, lotions, or powders applied to the skin for 2 to 4 weeks can usually treat an athlete’s foot (tinea pedis) and jock itch (tinea cruris). There are numerous non-prescription ringworm treatments available, including:
- Miconazole (Aloe Vesta Antifungal, Azolen, Baza Antifungal, Carrington Antifungal, Critic Aid Clear, Cruex Prescription Strength, etc.)
- Terbinafine (Lamisil)
- Clotrimazole (Lotrimin, Mycelex)
- Ketoconazole (Xolegel)
Follow the instructions on the package label for creams, lotions, and powders that are not prescribed. In the event that your infection doesn’t go away or worsens, get in touch with your doctor.

- Ringworm on the scalp (tinea capitis) is typically treated with oral antifungal prescription medication for 1 to 3 months. Creams, lotions, or powders won’t treat ringworm on the scalp. For the treatment of scalp ringworm, the following prescription antifungal medications are used:
- Itraconazole (Onmel, Sporanox)
- Griseofulvin (Grifulvin V, Gris-PEG)
- Terbinafine
- Fluconazole (Diflucan)
Home Remedies for Ringworm
Ringworm rashes are not serious, but they can be unsightly and embarrassing. Fortunately, there are several home remedies that can help treat and relieve the symptoms of ringworm.

One effective home remedy for ringworm is to apply tea tree oil to the affected area. Tea tree oil has antifungal properties that can help kill the fungus that causes ringworm. Simply mix a few drops of tea tree oil with a carrier oil, such as coconut oil, and apply it to the rash. Repeat this procedure several times per day until the rash has gone away.

Another remedy is to use garlic, which has powerful antifungal properties. Crush a few cloves of garlic and apply them to the rash. Leave it on for a few minutes, then rinse it off with water. Several times a day, repeat this procedure.

Another option is apple cider vinegar, which has antifungal properties and can help to dry out the rash. Apply a cotton ball soaked in apple cider vinegar to the rash. Allow a few minutes before rinsing with water. This procedure should be carried out several times a day.
Maintaining cleanliness and dryness in the affected area is also crucial. Avoid wearing tight-fitting clothing and opt instead for airy, loose clothing. Keep your personal items, like towels and clothing, to yourself. Keep your hair clean, and refrain from using hairstyling products like gels or sprays that can trap moisture if you have ringworm on your scalp.
Overall, since ringworm infections can take several weeks to completely clear up, it’s crucial to use these home remedies consistently. However, it is important to note that home remedies should not be used in place of medical treatment. If the rash does not respond to home remedies or gets worse, it is important to consult a dermatologist or other medical expert for proper diagnosis and treatment.
Is Ringworm Contagious?
Yes, ringworm is contagious and it can be spread through contact with an infected person, animal, or object. The fungus that causes ringworm can live on surfaces such as clothing, towels, or bedding. It can also be spread through skin-to-skin contact or by sharing personal items such as combs or brushes. In addition, people with weakened immune systems are at a higher risk of contracting ringworm.

It is important to practice good hygiene and avoid close contact with infected people or animals. If you think you may have been exposed to ringworm, it is important to see a doctor for diagnosis and treatment.
How does it spread?
Ringworm can spread through various ways, including:
- Direct contact with an infected person, animal, or object.
- Indirect contact with an infected person, animal, or object. For example, if you touch an object that has the fungus on it, and then touch your skin, you can develop ringworm.
- Direct skin-to-skin contact with an infected person, such as during sports or other activities that involve close physical contact.
- Sharing personal items such as combs, brushes, towels, or clothing with an infected person.
- Coming into contact with contaminated soil or surfaces, such as locker rooms or swimming pools.
It’s important to note that the fungus that causes ringworm can live on surfaces for several days, so it can be spread easily if not properly cleaned or sanitized.
From Cats and Dogs:
Ringworm can also be spread from cats and dogs. It is important to practice good hygiene when handling animals, as the fungus can be spread through contact with their fur, skin, or saliva. It is also important to keep cats and dogs clean and well-groomed to reduce the risk of infection.
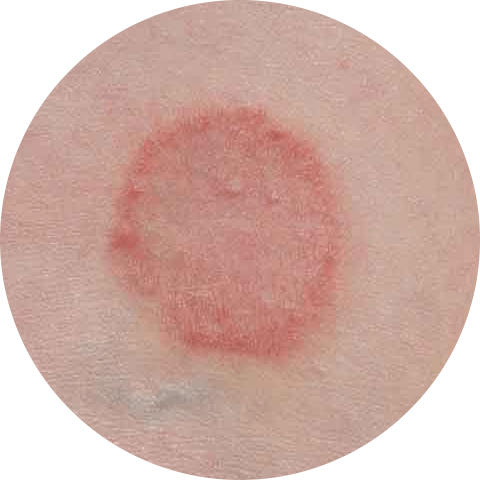
Ringworm vs. Eczema
Ringworm and eczema are two common skin conditions that can cause red, itchy, and scaly rashes. While they have some similarities, they are caused by different factors and require different treatments.
Ringworm is a fungal infection caused by a group of fungi known as dermatophytes. It typically appears as a ring-shaped rash with a red, scaly border and a clear center. Ringworm is highly contagious and can be spread through direct or indirect contact.
Eczema, also known as atopic dermatitis, is a chronic skin condition that causes an itchy, red rash. Eczema is not contagious and is caused by a combination of genetic and environmental factors. It is often associated with allergies and asthma, and can be triggered by irritants such as soaps and detergents.
The treatment for ringworm and eczema is very different. Ringworm is typically treated with topical or oral antifungal medications. Eczema can be treated with a combination of medicated creams and ointments, moisturizers, and lifestyle changes. In some cases, a doctor may recommend phototherapy or immunomodulators.
In summary, ringworm and eczema are two different skin conditions that can have similar symptoms. However, ringworm is caused by a fungal infection and is highly contagious, while eczema is caused by a combination of genetic and environmental factors and is not contagious. For accurate diagnosis and treatment, it’s crucial to see a doctor.
Ringworm vs. Psoriasis
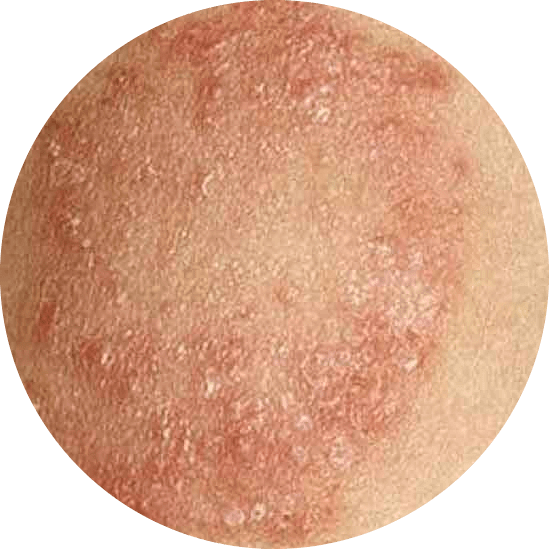
Ringworm and psoriasis are two skin conditions that can cause red, itchy, and scaly rashes, but they are caused by different factors and require different treatments.
Ringworm is a fungal infection caused by dermatophytes, a type of fungus. It looks like a ring-shaped rash with a red, scaly border and a clear center. Ringworm is extremely contagious and can be transmitted through either direct or indirect contact.
Psoriasis is a chronic autoimmune condition that causes skin cells to grow and reproduce at an accelerated rate. This results in the buildup of dead skin cells on the surface, known as plaques. These plaques can appear anywhere on the body but are commonly found on the scalp, elbows, and knees.

Ringworm and psoriasis are treated differently. Ringworm is typically treated with antifungal topical or oral medications, whereas psoriasis is treated with a combination of topical medications, phototherapy, and, in some cases, oral or injectable medications to suppress the overactive immune response.
In conclusion, ringworm and psoriasis are two different skin conditions with similar symptoms. Ringworm, on the other hand, is caused by a fungal infection and is highly contagious, whereas psoriasis is a chronic autoimmune disease. It is critical to see a doctor for a proper diagnosis and treatment.
Prevention Tips for Ringworm
To prevent ringworm, it is important to practice good hygiene and to avoid sharing personal items with others. Here are some additional prevention tips:
- Keep your skin clean and dry. This will help to prevent the growth of fungus and reduce the likelihood of infection.
- Wear breathable clothing and avoid tight-fitting clothing that can trap moisture against the skin.
- Avoid sharing personal items such as towels, combs, and clothing with others.
- Keep your feet clean and dry, especially if you spend a lot of time in communal areas like locker rooms or public showers.
- Avoid walking barefoot in communal areas like swimming pools, gym locker rooms, and showers.
- Keep your nails trimmed and clean to prevent fungal growth.
- If you have ringworm, stay away from other people until the infection has been treated and cleared up.
- Clean and disinfect any surfaces that may have come into contact with the fungus, such as clothes, bedding, and towels.
- If you suspect that you have ringworm, see a healthcare provider for an accurate diagnosis and treatment.
It’s worth noting that, while ringworm is highly contagious, it’s also highly treatable with antifungal medications. However, it is critical to take precautions to avoid spreading the infection to others. In addition, if you have a weakened immune system, you should take extra precautions to avoid ringworm exposure and seek medical attention if you suspect you have an infection.
How to Diagnose Ring worm
Ringworm can be difficult to diagnose because its symptoms can mimic those of other skin conditions. However, there are several methods that can be used to diagnose ringworm, including:
- Physical examination: A healthcare provider will examine the affected area of skin and look for characteristic signs of ringworm, such as a red, scaly, and itchy rash.
- Microscopic examination: A sample of skin, hair, or nails may be taken and examined under a microscope to look for the presence of fungal spores.
- Skin culture: A sample of skin can be taken and grown in a lab to confirm the presence of the fungus that causes ringworm.
- Wood’s lamp test: This test uses a special type of ultraviolet light to make fungal spores fluoresce, making them easier to see.
In addition to these diagnostic methods, a healthcare provider may also ask questions about a person’s medical history, symptoms, and risk factors for ringworm to help make a diagnosis. It’s important to see a healthcare provider if you suspect you have ringworm. A proper diagnosis is essential for effective treatment and to prevent the spread of infection to others.
When to See a Doctor for Ringworms?
Ringworm is a highly treatable fungal infection, but it is important to seek medical attention if you suspect you have it. If you have any of the following signs or symptoms, you should see a healthcare provider as soon as possible:
- A red, scaly, and itchy rash on the skin, scalp, nails, or feet
- A circular or ring-shaped rash
- Blisters or pustules on the skin
- Scaling or flaking of the skin
- Cracking or discoloration of the nails
- Hair loss or thinning on the scalp
- Itching, burning, or pain on the affected area
- If you have a weakened immune system, it’s also important to seek medical attention if you suspect you have a ringworm infection, as it can lead to more severe symptoms and complications.

Additionally, if the over the counter treatments doesn’t work, it’s always a good idea to see a healthcare provider for a proper diagnosis and treatment. Ringworm can mimic other skin conditions, so it’s important to get a proper diagnosis in order to receive the most effective treatment.
You can get more information about online dermatology consultation by click on the link.
Conclusion
In conclusion, ringworm is a common fungal infection that affects the skin, scalp, nails, and feet. It is characterized by a red, itchy rash and is most commonly transmitted through direct skin-to-skin contact with an infected person or animal. Topical antifungal medications are often effective in treating mild ringworm, but more severe infections may require antifungal pills for several weeks. To prevent ringworm, it is important to practice good hygiene, avoid sharing personal items with others, and to keep the affected area clean and dry. If you suspect you have ringworm, it is important to see a healthcare provider for an accurate diagnosis and treatment. With proper care, ringworm can be effectively treated and prevented.

2 comments
Can ringworm affect internal organs, or is it limited to the skin?
Thank you for your comment and question about ringworm. Ringworm is typically limited to the skin, scalp, and nails, and does not affect internal organs. However, in rare cases, it can lead to complications such as bacterial infections that can affect internal organs.