Atopic dermatitis, also known as eczema, is a chronic skin condition that causes inflammation, itching, and other symptoms. It can affect both children and adults and is often associated with atopy, a group of disorders that includes eczema, asthma, and allergic rhinitis. People with atopic dermatitis may have high levels of a type of antibody called immunoglobulin E (IgE) and may have a family history of atopy.
While exposure to allergens may be linked to atopic dermatitis in some cases, it is not necessarily a direct cause of the condition. However, it may contribute to the severity of the disease in some patients.
This post will provide a detailed overview of atopic dermatitis, including its causes, symptoms, different types, treatment options, and prevention methods.
What is Eczema?
Eczema is a long-term skin condition that causes inflammation, itching, dryness, rashes, scaly patches, blisters, and skin infections. It is most commonly characterized by itchy skin, and there are seven types of eczema: atopic dermatitis, contact dermatitis, dyshidrotic eczema, nummular eczema, seborrheic dermatitis, and stasis dermatitis.
Approximately 31 million Americans have eczema, which can appear at any age but is most common in young children, adolescents, and adults over the age of 50. Severe eczema can cause flare-ups that last for several days or weeks.
Treatment options for eczema include moisturizers, antihistamines, topical steroid creams, light therapy and oral medications, as recommended by skin doctors, dermatologists… It is important to get a proper diagnosis as eczema can be mistaken for other skin conditions like psoriasis. A dermatologist or other qualified healthcare professional can help develop a symptom management plan and prevent future flare-ups.
What are the underlying causes of Eczema?
Eczema, also known as atopic dermatitis, is a skin condition caused by an overactive immune system that reacts to irritants or allergens on the skin. According to the American Academy of Dermatology, atopic dermatitis is a complex skin disease that results from a combination of genetic and environmental factors.

People with atopic dermatitis may have a gene variation that affects the skin’s ability to provide protection. This can lead to a compromised barrier function, which makes the skin less able to retain moisture and defend against bacteria, irritants, allergens, and other environmental factors like tobacco smoke.

In some cases, an overgrowth of the bacteria Staphylococcus aureus on the skin may also cause atopic dermatitis by disrupting the skin’s barrier function and triggering an immune response.
There are several types of dermatitis, including atopic dermatitis (eczema), contact dermatitis, and seborrheic dermatitis (dandruff).
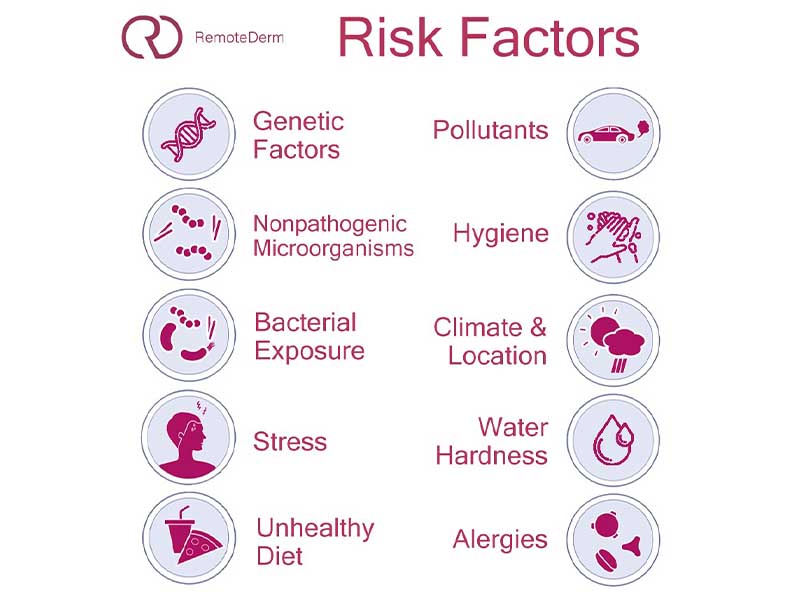
Eczema Risk factors
Atopic dermatitis risk factors include a variety of genetic and environmental factors, including:
Genetic risk factors
One of the strongest risk factors for atopic dermatitis is a family history of atopy, which includes eczema, asthma, and allergic rhinitis. Approximately 70% of patients with atopic dermatitis have a positive family history of atopic diseases. Children with one parent who has atopy have a two to three times greater risk of developing atopic dermatitis, and if both parents have atopy, the risk increases to three to five times greater.

Loss-of-function variations in the FLG gene, which cause a faulty epidermal barrier, are a major risk factor for atopic dermatitis and other skin and allergic conditions such as allergic contact dermatitis, asthma, and food allergies. Other genes that may play a role in the development of atopic dermatitis include those involved in regulating innate host defenses and T-cell function.
Environmental exposures
There are several environmental factors that may increase the risk of atopic dermatitis, including climate, location (urban or rural), air pollution, early exposure to nonpathogenic microorganisms, and water hardness. Some studies have linked these factors to the development of atopic dermatitis.
- The “hygiene hypothesis”
According to two systematic reviews, there is evidence to suggest that early daycare, helminth infestation, having a large number of siblings, exposure to farm animals, and having a pet dog may be protective against atopic dermatitis. On the other hand, viral or bacterial infections do not seem to have a protective effect.
- Water hardness
According to a meta-analysis of seven observational studies involving nearly 386,000 participants, there may be a slight increase in the risk of atopic dermatitis in children exposed to hard water. However, the authors of the study noted that the reliability of this estimate is very low due to the high risk of bias and differences in the definition of “hard water” across the studies.
Eczema triggers
Eczema triggers are factors that can cause or worsen eczema symptoms, regardless of the underlying cause of the condition. It is important to note that eczema flare-ups can occur some time after exposure to irritants or allergens, and it may be difficult to identify certain triggers due to this delay.
A variety of factors could be causing your eczema symptoms. These will differ from person to person. Typical triggers include:
- Irritants, including shampoo, dishwashing liquid, and bubble baths as well as soaps and detergents.
- Dry skin: If your skin becomes excessively dry, it may become brittle, scaly, rough, or tight, which can increase the risk of an eczema flare-up. To manage severe eczema flare-ups, it is important to keep your skin moisturized with ointments and creams that are formulated for use on eczema-affected skin. This can help to reduce the risk of dryness and irritation.
- Environmental factors or allergens, such as cold and dry weather, dampness, and more specific things like house dust mites, pet fur, pollen, and mold.
- Food allergies, including those to wheat, soy, cow’s milk, eggs, peanuts, and other common foods, are very prevalent.
- Specific materials in contact with the skin, like wool and synthetic fabrics
- Hormonal changes: women’s symptoms may worsen in the days leading up to their period or during pregnancy.
- Stress: It is unknown why emotional stress can cause eczema. When people are “stressed,” their eczema symptoms worsen. Others may become stressed simply by knowing they have eczema, which can aggravate their itchy skin.
- Skin infections
Some people with eczema may find that their symptoms worsen when the air is dry or dusty, or when they are sweaty, too hot, or too cold. This can create a cycle in which stress leads to worsening eczema symptoms, which in turn can cause more stress. To break this cycle, it may be helpful for these individuals to learn stress management techniques. This can help to reduce the impact of stress on eczema symptoms and improve overall quality of life.

Is eczema contagious?
No, eczema is not contagious, meaning it cannot be spread from person to person. If you think you have developed a rash due to contact with someone else, it is not likely to be eczema. However, it is important to note that eczema can cause broken skin, which may be susceptible to contagious infections. To reduce the risk of infection, it is important to protect any open wounds or areas of cracked skin if you have eczema.
Common Symptoms of Eczema
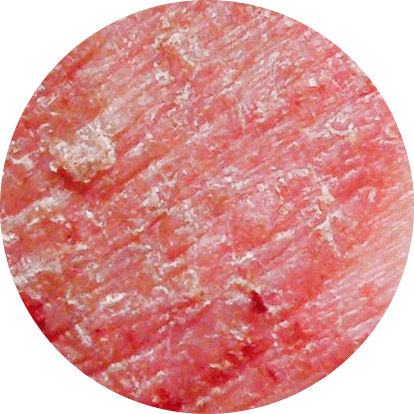
Eczema, also known as atopic dermatitis, is a skin condition characterized by dry skin and intense itching. Other common symptoms may include inflammation, rash, scaling, redness, cracking of the skin, and fluid oozing. The appearance of eczema can vary greatly depending on the patient’s age, ethnicity, and disease activity.

Acute eczema is marked by inflamed, itchy, red papules and vesicles with exudation and crusting, while subacute or chronic lesions are characterized by dry, scaly, or excoriated inflamed papules. Chronic scratching can lead to skin thickening (lichenification) and fissuring. Many patients may have lesions in various stages present at the same time.
In individuals with deeply pigmented skin, erythema (skin redness) may appear dark brown or violet rather than pink or red, and the erythematous and scaly lesions of eczema may also appear grayish violet or dark brown. Dry skin in these individuals may be whitish or ashy in color and may have less shine.
7 Different Types of Eczema
Eczema can present with a wide range of presentations, depending on the specific type of eczema. Some common types of eczema include contact dermatitis, which is caused by contact with irritants or allergens, and seborrheic dermatitis, which often appears as yellowish, oily scales on the scalp. Each type of eczema has its own unique set of symptoms and triggers, which will be discussed in more detail below.

1. Atopic Dermatitis
Atopic dermatitis is a common type of eczema that usually begins in childhood and often improves or disappears in adulthood. It is part of the “atopic triad,” a group of three conditions that includes asthma and hay fever. Many people with atopic dermatitis also have one or more of these other conditions.

Symptoms
- The rash frequently develops in the creases of the knees or elbows.
- Babies are more likely to develop a rash on their cheeks and scalp.
- The skin surrounding the rash may thicken, lighten, or darken.
- If you scratch tiny bumps, fluid may leak from them.
- If you scratch your skin, an infection could develop.
Causes
Atopic dermatitis develops when your skin’s natural barrier against the elements is compromised. As a result, your skin is less capable of protecting you from irritants and allergens. Atopic dermatitis is most likely caused by a combination of factors, including:
- Genetics
- Skin dryness
- Issue with the immune system
- Environmental triggers
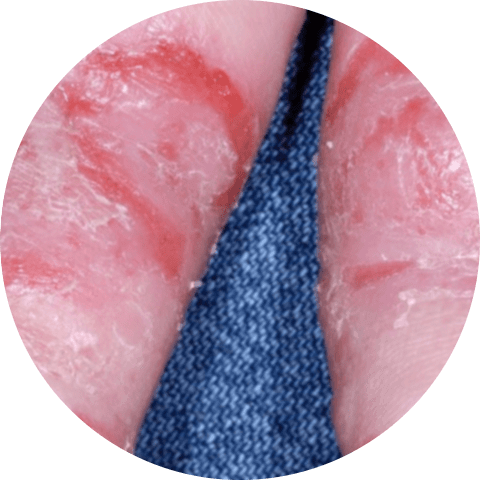
2. Hand Eczema
Simply put, hand eczema is a type of eczema that only affects your hands. You may develop this type if you work in a field where chemicals that irritate the skin are frequently used, such as hairdressing or cleaning.

Symptoms
- The skin on your hands becomes red, hyperpigmented, itchy, and dry.
- They may develop cracks or blisters.
Causes
Exposure to chemicals causes hand eczema. This form is more common in people who work in jobs that expose them to irritants, such as:
- Healthcare
- Dry cleaning or laundry
- Hairdressing
- Cleaning
3. Stasis dermatitis
Stasis dermatitis occurs when fluid leaks into your skin from weakened veins. This fluid is mainly responsible for:
- Swelling
- Redness in people with lighter skin tones
- Darker skin tones may be brown, purple, gray, or ashen.
- Itchiness
- Pain
Symptoms
- Your legs may feel achy or heavy.
- The lower part of your legs may swell, especially if you’ve been walking around all day.
- You will almost certainly have varicose veins, which are thick, ropey, damaged veins in your legs.
- Dry and itchy skin will develop over the varicose veins.
- You may develop open sores on the bottoms of your legs and the tops of your feet.

Causes
People who have poor blood flow to their lower legs can develop stasis dermatitis. Blood can pool in your legs if the valves that should push blood up through them and toward your heart aren’t working properly.
4. Contact dermatitis
If a region of your skin becomes red, inflamed, thick, or scaly and itchy after coming into contact with something, you may have contact dermatitis.

There are two kinds of it: An immune system reaction to an irritant, such as latex or metal, causes allergic contact dermatitis. When a chemical or other substance irritates your skin, irritant contact dermatitis develops.
Symptoms
- The skin may become thicker and more scaly or leathery over time.
- Skin itches, turns red, becomes hyperpigmented (or pink), turns magenta, burns, and stings.
- Hives, or itchy bumps, may appear on your skin.
- Blistering may develop that is liquid-filled, oozes, and crusts over.
Causes
When you come into contact with something that irritates your skin or sets off an allergic reaction, contact dermatitis develops. The most frequent causes include:
- Poison ivy and other toxic plants
- Makeup and skin care products
- Perfumes and soaps
- Detergents
- Bleach
- Jewelry
- Latex
- Nickel
- Paint
- Solvents
- Smoking tobacco
5. Dyshidrotic Eczema
Small blisters form on your hands and feet as a result of dyshidrotic eczema. It affects more women than men. These blisters can be intensely itchy and painful, leading to redness and swelling in the area.
Symptoms
- Blisters filled with fluid form on the fingers, toes, palms, and foot soles.
- These blisters can itch or hurt.
- Scales, cracks, and flakes can appear on the skin.
Causes
- Exposure to materials like chromium salt, nickel, or cobalt
- The use of tobacco products
- Allergies
- Damp hands and feet
- Stress
- Hand sanitizers
- Frequent handwashing
6. Neurodermatitis
Neurodermatitis is similar to. It causes your skin to develop thick, scaly patches. In addition, neurodermatitis is often characterized by intense itching, which can be very difficult to control.

Symptoms
- Arms, legs, the back of the neck, the scalp, the bottoms of feet, the backs of hands, or genitals develop thick, scaly patches.
- The patches can be extremely itchy, particularly when you’re relaxed or sleeping.
- If you scratch the patches, they can bleed and get infected.
Causes
People who already have eczema or psoriasis are more likely to develop neurodermatitis. Dermatologists aren’t sure what causes it, but stress may be a factor. Stressful situations, such as problems at home or at work, can make it worse.
7. Nummular Eczema
Round, coin-shaped spots appear on your skin as a result of this type of eczema. The spots are typically red and scaly, and they usually itch intensely. In Latin, the word “nummular” means coin. Nummular eczema differs from other types of eczema in appearance and itchiness.

Symptoms
- Round, coin-shaped spots
- The spots may become itchy or scaly.
Causes
Nummular eczema can be caused by an allergic reaction to an insect bite or an allergic reaction to metals or chemicals. Dry skin can also contribute to it.
If you have another type of eczema, such as atopic dermatitis, you are more likely to develop the nummular variation.
What are Eczema treatment options?
Treatment options include lifestyle changes, over-the-counter (OTC) remedies, and prescription medication, depending on the type of eczema and its severity. Eczema symptoms can vary from person to person. Because not everyone responds the same way to the same treatment plan, it’s best to become acquainted with all of your options and consult with your healthcare provider to find a treatment regimen that works for you or your child.

The best management of atopic dermatitis usually requires a multifaceted strategy that includes the elimination of aggravating factors, hydration and restoration of the skin’s barrier function, patient education, and pharmacologic management of skin inflammation.
The following are the most common eczema treatment options:
- The itch can be relieved with antihistamines such as diphenhydramine (Benadryl).
- A cream or ointment containing corticosteroids can ease itching. You can take oral steroids like prednisone (Rayos) to reduce swelling if the reaction is more severe.
- Calcineurin inhibitors like tacrolimus (Protopic) and pimecrolimus (Elidel) lessen the immune response that causes itchy skin.
- Skin infections are treated with antibiotics.
- Your skin is exposed to ultraviolet light as part of light therapy to treat your rash.
- Applying cool compresses before applying corticosteroid cream can help the medication absorb more easily into your skin.
- Colloidal oatmeal can be used in lotions or baths to soothe itching.
- Moisturizing creams can help lock in moisture and reduce skin irritation.
- New medications including Dupixent can be beneficial
If an allergic reaction causes a flare-up of your eczema, you should avoid the offending substance. Other potential treatments for eczema include nonprescription medications and home remedies.
If you or a loved one is dealing with persistent eczema symptoms, consulting a dermatologist is crucial for effective management. At RemoteDerm, our experienced dermatologists specialize in diagnosing eczema accurately and recommending tailored treatments. Don’t let eczema disrupt your life; get an online consultation with our experienced dermatologists in Canada to explore eczema prescription treatments and regain control over your skin.
Suggestions for reducing outbreaks
Here are some tips for preventing eczema flare-ups and managing symptoms:
- To form a protective barrier against the elements, moisturize your skin daily with a rich, oil-based cream or ointment. To seal in moisture, apply the cream right after you get out of the shower or bath.
- To relieve the itch, apply cool compresses to your skin or take a colloidal oatmeal or baking soda bath.
- After bathing, pat your skin gently with a soft towel. Never, ever rub.
- Scratching should be avoided. You may spread infection.
- Use fragrance-free detergents, cleansers, cosmetics, and skincare products.
- Always wear gloves and protective clothing when handling chemicals.
- Dress comfortably in loose-fitting clothing made of soft materials, like cotton.
Eczema Prevention
Eczema is a chronic condition whose severity varies, sometimes improving and sometimes worsening. Some people can go years without showing any signs of illness. It is not curable, but the symptoms can be managed with moisturizers, topical and oral medications, and self-care measures. The following are some preventative measures for eczema flare-ups:
Skin barrier enhancement
The dysfunction of the epidermal barrier is recognized as a key factor in the onset and progression of atopic dermatitis. Certain plant oils may help repair the skin barrier while also preventing moisture loss. Antibacterial, anti-inflammatory, and antioxidant properties are present in many of these oils. Jojoba, coconut, almond, and argan oils are some of the most effective plant oils to use on your skin.
Probiotics and dietary supplements
Lactobacillus-containing probiotics appear to be of limited benefit in terms of symptom improvement. There is also conflicting evidence for the use of probiotics to prevent eczema in high-risk children.
Supplements such as vitamins, fish oil, and evening primrose oil appear to have limited efficacy evidence.
Avoiding Trigger Factors
Heat (overheating of the skin), perspiration, and a dry environment are all triggers. Eczema can also be triggered by emotional stress or anxiety. Chemicals (such as soaps, detergents, perfumes, or cosmetics), materials (such as wool or synthetic fibers), dust, sand, and smoke can all cause a flare-up. It may take some effort and time to identify the trigger factors, but avoiding such factors is critical for long-term control of the condition.
By click on the link, you can get more information about online dermatology consultation in Remotederm.
Eczema FAQs
1. What should I expect from living with Eczema?
Eczema and other types of dermatitis are not harmful to your overall health. The condition is not fatal. By the time they reach puberty, nearly half of children with eczema have outgrown it or improved. Others will have some form of the condition for the rest of their lives. A good skincare routine can help adults with eczema manage their condition.
2. Does the weather aggravate Eczema?
Yes, certain temperatures or weather patterns can have an effect on your skin and aggravate eczema. Low humidity (dry air) in the winter months can cause skin dryness. High humidity can cause you to sweat, which can aggravate your itchiness.
Dandruff is a condition in which dry skin flakes off the scalp. Eczema is a chronic, inflammatory skin condition that is frequently linked to allergies. Flakes are a common symptom of eczema. However, dandruff and eczema are not the same.
Bottom Line
Eczema is a skin condition characterized by dry, itchy patches of skin. It’s a common, non-contagious condition. If you come into contact with an irritant or allergen, your eczema symptoms may worsen. There are treatments to help you manage your symptoms, but there is no cure. On top of that, there are prevention methods that individuals can take to manage symptoms of Eczema.

If you have symptoms of Eczema, contact a skin dermatologist to determine the best method of prevention and treatment for your own specific type of eczema. We suggest you to click on the link and read another article to get more information about skin dermatologist in Remotederm.

6 comments
Can eczema be caused by a reaction to certain medications or chemicals in products?
Yes, certain medications and chemicals in products can cause a reaction that leads to eczema. This is known as contact dermatitis, a type of eczema caused by exposure to an allergen or irritant.
This article has been helpful in explaining the underlying causes of eczema, but what are some effective treatment options for someone with severe eczema?
Treatment for severe cases of eczema may involve prescription medications such as corticosteroids, immunosuppressants, or biologic drugs. In addition, light therapy or wet dressings may also be recommended by a dermatologist. It’s important to consult with a dermatologist to determine the best treatment plan for your specific condition.
Hi! can you recommend any specific products or ingredients to look for in skincare products for eczema-prone skin?
Look for products that contain ceramides, which are natural lipids found in the skin’s outer layer that help maintain the skin barrier. Also, avoid products with fragrances, dyes, and other potential irritants.